July 08, 2025

For three decades, H.H.C. Group has gone head-to-head with inflated claims, aggressive providers and shifting regulations to do one thing: protect payors' bottom lines. As of July 1, 2025, that fight has been going strong for 30 years — and we're just getting started.
What began in 1995 as a focused out-of-network negotiation firm has grown into one of the most trusted cost-containment partners in the country. Serving self-insured plans, TPAs, stop-loss carriers, unions and state governments, H.H.C. Group delivers unmatched clinical, legal and negotiation expertise.
30 Years of Staying Power — Built on Performance
In this industry, longevity doesn't come easy. It takes relentless focus, deep expertise and the discipline to challenge inflated charges and deliver outcomes where others fall short.
We Do the Hard Work Others Won't
Cost pressures on payors are intensifying. Claims are higher, provider tactics more aggressive and billing systems increasingly complex. H.H.C. Group brings precision, speed and accountability to every case — no matter how large or layered. And at the heart of all? Real people with real expertise.
From multi-million-dollar inpatient stays to excessive pharmacy claims and complex compliance issues, we step in where others stall out. Fast. Precise. Relentless.
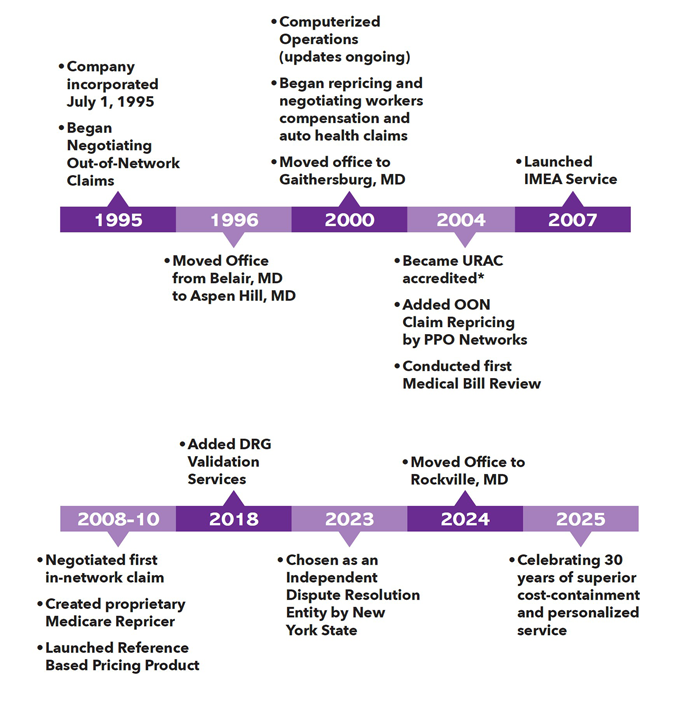
30 Years of Milestones and Forward Momentum
H.H.C. Group has grown by staying sharp and staying in front of every shift in the healthcare market. The timeline says it all:
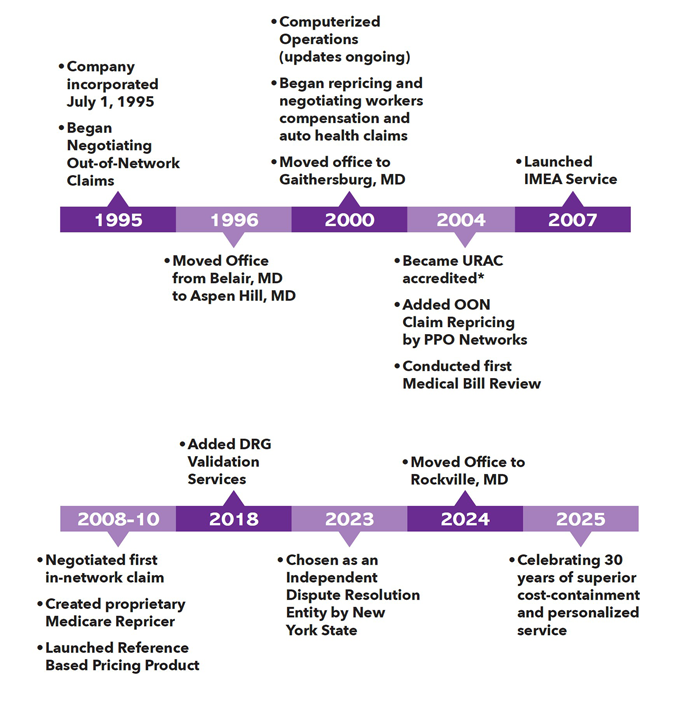
*Successfully reaccredited every 3 years since 2004
We Don't Just Respond — We Lead the Charge
H.H.C. Group has built the strategy, infrastructure and team to push back against upcoding, inflated charges and provider delay tactics — and win.
- High-Dollar Claims Negotiation:
Attorney-led negotiations that cut through red tape and reduce inflated claims by up to 90%, with signed provider agreements to eliminate balance billing.
- Out of Network Claim Repricing:
National, regional, and local networks combined with intelligent claim routing and repricing—down to the last dollar—to maximize every savings opportunity.
- Independent Medical Reviews (IMRs):
URAC-accredited, state-approved, and clinically sound—H.H.C. Group is trusted to deliver objective, evidence-based decisions that hold up under scrutiny.
- Line-Item and Comprehensive Medical Bill Reviews:
Our clinical and coding experts conduct both detailed line-item reviews and full medical record-level audits to identify inaccuracies, inappropriate charges, and hidden errors that others miss.
- Reference-Based Pricing (RBP):
Transparent, defensible pricing aligned with Medicare benchmarks ensures fairness and cost control in high-stakes claims.
- Compliance and Legal Strength:
We understand the regulatory frameworks inside and out — and we don't blink when things get complicated.
What Payors Need to Know
In today's environment, hesitation is costly. Unchecked claims and delayed decisions erode your margins — and providers are counting on it. You need a partner who moves fast, enforces standards and delivers real results from real people.
Our seasoned team of professionals bring unmatched clinical insight, legal strategy and cost-containment expertise that hold up under pressure.
Take the Next Step
The pressure isn't letting up — and neither are we.
Contact HHC Group to take control of rising claim costs. With the tools, talent and tenacity to cut through complexity, we help payors stay aggressive, stay compliant and stay ahead.
Real Oversight. Real Control. Real People. Real Savings.